Despite great advances in genetics and modern imaging, the diagnosis of breast cancer takes most patients by surprise. For some, it comes too late. Late diagnosis means aggressive treatments, uncertain results and more medical expenses, which is why the detection of patients has been a central pillar of the investigation of the disease that, it is estimated, will have 300 thousand 590 new cases this 2023, and will claim lives of 43 thousand 700 people.
With that in mind, a team from the Computer Science and Artificial Intelligence Laboratory ?CSAIL? of the Massachusetts Institute of Technology ?MIT? and Massachusetts General Hospital ?MGH?, has created a new deep learning model where Artificial Intelligence helps predict cancer, from a mammogram, if a patient is likely to develop breast cancer up to five years in the future.
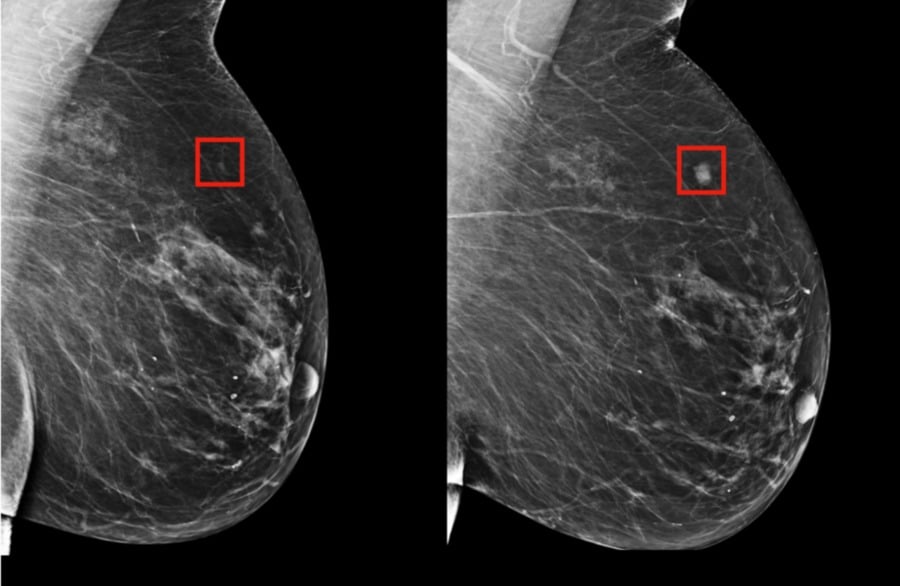
Trained on mammograms and known results from more than 60,000 MGH patients, the model learned the subtle patterns in breast tissue that are precursors to malignancies.
MIT professor Regina Barzilay, a breast cancer survivor, says the hope is that systems like these allow doctors to customize screening and prevention programs on an individual level, making late diagnosis a relic of the past.
Although mammography has been shown to reduce mortality from breast cancer, there is an ongoing debate about how often to get screened and when to start.
While the American Cancer Society recommends annual screening starting at age 45, the US Prevention Task Force recommends screening every two years starting at age 50.
"Instead of taking a one-size-fits-all approach, we can customize screening based on a woman's risk of developing cancer," Barzilay said. "For example, a doctor might recommend that one group of women have a mammogram every two years, while another higher-risk group might have a complementary MRI."
Barzilay is Professor of Delta Electronics at CSAIL and in the Department of Electrical Engineering and Computer Science at MIT and a member of the Koch Institute for Integrative Cancer Research at MIT.
The team's model was significantly better at predicting risk than existing approaches: it accurately placed 31 percent of all cancer patients in their highest-risk category, compared with just 18 percent for traditional models.
How does it work
Since the first breast cancer risk model in 1989, development has been driven largely by human knowledge and intuition of what the major risk factors might be, such as age, family history of breast cancer, and ovary, hormonal and reproductive factors and breast density.
However, most of these markers only weakly correlate with breast cancer. As a result, such models are still not very accurate at the individual level, and many organizations continue to feel that risk-based screening programs are not possible given these limitations.
Instead of manually identifying the patterns in a mammogram that lead to future cancers, the MIT/MGH team trained a deep learning model to infer the patterns directly from the data. Using information from more than 90,000 mammograms, the model detected patterns too subtle for the human eye to detect.
More equitable detection of cancer
The project also aims to make risk assessment more accurate for racial minorities, in particular. Many of the early models were developed on white populations and were much less accurate for other races.
Meanwhile, the MIT/MGH model is equally accurate for white and black women, which is very important given that the latter have been shown to be 42 percent more likely to die of breast cancer due to a wide range of reasons. factors that may include differences in detection and access to care.
Barzilay says his system could also one day allow doctors to use mammograms to see if patients are at higher risk for other health problems, such as cardiovascular disease or other cancers.
The researchers are eager to apply the models to other diseases and conditions, and especially those with less effective risk models, such as pancreatic cancer.
You may be interested in: San Mateo County invested more than $360 million in aid during the COVID-19 pandemic


